Whether or not you have children, you are probably familiar (at least a little) with an epidural for labor. And if you’re pregnant right now, my guess is you may have an idea of whether or not you’d like to use one. Regardless of where you are in your decision-making process, let’s answer the questions:
- What is an epidural?
- What does an epidural do?
- How does an epidural work?
- What are the risks and benefits of an epidural?
- What is it like to get an epidural?
Hopefully, this information will help you make a decision (or affirm the decision you’ve already made) about an epidural for labor.
What is an epidural during childbirth?
An epidural is a “regional” form of pain control for labor. This means the medication is meant to work in a specific location without impacting the entire body. Epidurals, spinals, and combined spinal-epidural anesthesia (CSE) are meant to provide pain relief to the midsection of the body. The medication should decrease the level of contraction and perineal/vaginal pain you are feeling.
In the US, more than 60% of laboring people receive an epidural, spinal, or CSE. Epidurals during labor are placed by an anesthesiologist or a certified registered nurse anesthetist (CRNA). These medical “blocks” work by putting anesthesia medication into the space around the spinal nerves in your lower back. This stops contraction pain signals from traveling from your spine to your brain.
How long does an epidural for labor last?
An epidural delivers continuous medication and is the most common block used for labor. The medication delivers pain relief to you until your baby and your placenta have delivered. The epidural medicine does not run out or stop working, though things can feel different as labor progresses.
A spinal block is more common for a cesarean delivery – it only works for about 2 hours. A CSE, also called a walking epidural, combines the action of the spinal and the epidural. It offers rapid pain relief from the spinal dose along with the continuous action of the epidural, and it can be used throughout labor.
When to get an epidural during labor?
There is no perfect time to request an epidural. The “right” time to receive one will be based on a lot of things. This includes your pain tolerance and preferences, what stage of labor you are in, and how you are handling what is going on.
As an RN, I think the best time to get an epidural is as you move into active labor. At this point in labor you are probably:
- consistently contracting
- experiencing cervical change
- able to “control” yourself during contractions
- about 4-6 cm dilated
- not feeling an urge to push
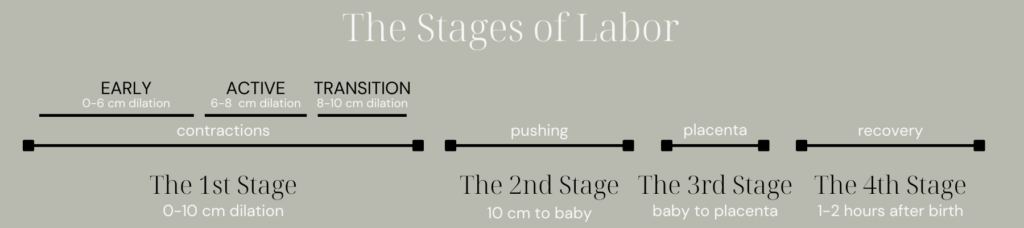
If you are feeling an urge to push, you may have already moved into the transition phase of labor. While this does not mean you cannot have an epidural for labor, there may not be enough time to get you one. If this is your 2nd or 3rd+ baby, there’s an even greater chance that it is too late.
What if I want an epidural earlier?
Sometimes, patients request an epidural before they are in the active phase of labor. Many of my patients have received one long before they are 4 centimeters! There is not a firm rule about when you are “allowed” to have one. If you want one earlier in the process, chat with your nurse about it. They can help you decide the best time, assist you with other pain management tools, and connect you with your doctor or midwife if you want their opinion too.
Alternatively, you may hear that “you cannot have an epidural after you are 8 cm dilation.” This is not true. If you can hold still and baby is not crowning, you can receive an epidural for labor. I have had many patients ask for and receive an epidural in the middle of a couple of hours of pushing! But overall, if you ask for an epidural later in the process, there are times when your labor will be moving too fast for you to get one.
What are the benefits of an epidural for labor?
An epidural can offer a variety of benefits. In many different studies, it has been shown to be the most effective form of pain relief. When compared to IV pain medication, epidural anesthesia is also safer. This is because it does not cross the placenta in the same ways. Anecdotally, epidurals offer more opportunity to rest and relax in labor. This may encourage cervical dilation, because a relaxed body often equals a more relaxed pelvic floor. The rest can also prove valuable for someone who needs energy and stamina for the second stage of labor – pushing!
What are the side effects of an epidural?
As with any anesthesia medication, an epidural does have potential side effects. Your anesthesia provider will detail these to you when you sign a consent with them before the placement. But let’s walk through them here so they sound familiar.
- A drop in blood pressure is one of the most common side effects after epidural placement. This can make you feel light headed or nauseous and change the oxygenation status of the baby. You may also need additional IV fluids or medications to correct the drop in BP.
- Temporary issues going pee after birth can also occur with an epidural. Typically, you have a urinary catheter placed after epidural placement, since the anesthesia causes a loss of bladder sensation. When the catheter is removed and you need to empty your bladder, there can be some retention until your bladder “wakes up.”
- There is a Cochrane review that also reports more fevers in those who labored with an epidural. These fevers may occur in 15-25% of those who receive an epidural. It’s believed that the anesthesia causes some sort of inflammatory response and affects the maternal body’s thermoregulation systems. If these fevers do show up, they are usually mild and can be treated with Tylenol. The epidural’s effect on the thermoregulation system can cause an increase in shivering too.
- Shivering can also be a result of hormonal changes during labor, so don’t be too surprised if you find that you develop the shakes! Itching after epidural is also possible, though this usually resolves as soon as the epidural is turned off and the medication leaves your body.
- Epidurals can slow down labor. The Cochrane review I mentioned also found that those with epidurals had longer first and second stages of labor, and were more likely to need Pitocin augmentation.
- Sometimes, it is reported that epidurals may increase the need for instrumental delivery with a vacuum or forceps. However, if one only analyzes data from after 2005, the increased risk actually no longer exists. This risk may not be true with today’s epidurals and their use.
Rare side effects of epidurals for labor
There are two more side effects that your anesthesiologist will mention to you: a spinal headache and anesthesia that moves too high. These situations are both rare, but they are real. A spinal headache occurs when spinal fluid leaks into the epidural space during insertion. The leak changes the pressure in your brain and causes a NASTY headache. The headache may resolve on its own or with certain medications, but occasionally, you need an additional procedure called a blood patch. The other side effect I mentioned is related to the level of anesthesia in your body. Typically, it moves no higher than the top of your belly. However, (rarely) the anesthesia can move too high, and you can end up feeling like you can’t breathe. This feeling can be reversed, but it’s scary when it happens!
Lastly, I want to affirm that epidurals have not been shown to increase the risk of cesarean birth or long-term back ache. These two things are commonly floated around in this discussion, but so far evidence does not show them to be true. Epidurals can certainly be part of births that end up in these situations, but they have not been shown to cause either.
Who cannot have an epidural for labor?
There are a few reasons you may not be able to have an epidural. This includes:
- low platelets
- an unstable baby
- a crowning baby
- the inability to sit still
- (sometimes)previous spinal surgery or scoliosis.
Your platelets are important for blood clotting. Their levels will get checked prenatally and when you are admitted for labor. If you have existing spinal concerns, bring them up prenatally! You can meet with a member of the anesthesia team before your birth, discuss your imaging together, and make a plan. The stability of the baby really can’t be planned. When delivery is needed really quickly, there just isn’t time for epidural or spinal placement and you’ll be put under general anesthesia. If your baby is crowning, get ready to meet them! And then sitting still will really be about you. The placement time is usually about 10 minutes, and a few of those minutes will require that you sit very still.
The epidural process: from request to relief
I want to give you a brief overview of the epidural process. While it may look a bit different at your birthing facility, you can likely expect all of this to be some part of it.
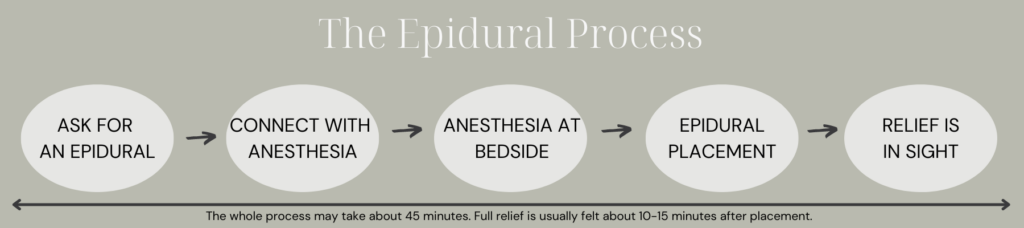
- You ask for your epidural: Your RN will need to make sure you have IV access and that your blood has been drawn and resulted (with those platelets)! Labs can have a turnaround time of about 30 minutes, so just know that if you’re asking for one the minute you are admitted. Your RN will likely start a fluid bolus as well – usually 500ml -1L of fluids is preferred to be in your body before anesthesia placement. A blood pressure cuff is placed as well, and an initial BP is taken.
- Connect with anesthesia: When you are prepped and your lab results are confirmed, anesthesia will be on their way. They are usually pretty prompt, though they can be delayed in the OR or working on other epidurals. Occasionally, some hospitals have to call an anesthesia person in from home.
- Anesthesia at the bedside: The anesthesia team member will go over risks with you and have you sign consent. They may ask your partner to leave the room – so know that this discussion might come up. They will then position you for the procedure. This is usually you dangling on your bed, often curved around a pillow. You will want to be relaxed, chin to chest, and curled up like shrimp. Usually a nurse or your partner can be standing or sitting in front of you.
- Epidural placement: The procedure is sterile, so you do need to stay still for a few reasons. Your back will be cleaned and it will feel cold. You will then feel a big pinch and sting when they give you local anesthetic in your back. When you are numb, the anesthesiologist will use a new, different needle to find the right space in your back. You may feel pressure at this point, but not pain. In these minutes, you do need to stay very still – even if a contraction occurs! Hopefully, the placement occurs quickly, but I have seen it take 5-10+ minutes. When your anesthesiologist has the needle in the right place in your back, they place a small catheter – like a tiny tube – through that needle and down into the epidural space. Sometimes, you will feel a “zing” down one of your legs – you can go ahead and let them know if you do. The needle is then removed and the catheter stays in! The anesthesiologist will administer a test dose of medicine to confirm the catheter is in the right place and then tape the catheter very well to your back.
- Relief is in sight: If your anesthesiologist has done a combined spinal-epidural, you will feel pain relief right away. If you have had a traditional epidural, which most do, it can take about 15 minutes to feel the fullness of relief. With your RN, the anesthesiologist will lay you back down and connect the catheter to your continuous medication. Usually, contractions start to feel shorter and shorter and less intense – until the associated pain is gone!
I detail the entire epidural process in my birth course, Your Body, Your Birth. Join me (and hundreds of other mamas) there for nearly 10 hours of video education. I’ll walk your through your pregnancy, your labor, your birth, and postpartum. It’s affordable, it’s on-demand, and it’s yours for life.
Extra notes about epidurals for labor
- Epidurals are intended to take away pain – not pressure. It’s okay if you still feel something! One of our CRNAs says “If your pain is 10/10, the epidural will bring it to a 3/10.” He wants you to understand that you may still feel something – but it’s usually pressure – and that does not mean it isn’t working.
- Sometimes, epidurals start working more on one side or another. This can often be adjusted with your position, as the medication does work with gravity. Let your RN know if this happens.
Some epidural machines also have a PCEA push button. This is a little clicker that allows you to administer extra medication to yourself. You are still getting continuous medication and you can’t overdose yourself. If you have one to use, it should be explained to you further. - There are times when you may need a bolus of extra medication again from the anesthesiologist. If you are feeling pain and are unsure – please speak up. It can mean lots of things (including something great like complete dilation!), but your RN needs to know.
- Typically, epidurals are a continuous infusion that stays on through the delivery of the baby and the placenta. If the bag of medication runs out, your RN or anesthesiologist can replace it. The anesthesia should also keep you comfy for any repairs that are needed after birth. The epidural will be turned off after the repair, and the catheter is often removed when you get out of bed a couple of hours later.
- Oftentimes, providers won’t let you eat or drink anything after you have an epidural placed. You can read more about being free to eat and drink during labor (or not) here.
The takeaway on epidurals for labor
I believe in the good and important use of epidurals in a variety of birth stories. I have seen them be a fundamental part of hundreds and hundreds of births. No one can tell you whether you should or should not get an epidural. This is YOUR choice – and you have autonomy in how and when to make this choice! If there is stigma attached to these – and I think there can be – I really want you to let it go. Don’t allow a narrative of how it is “supposed” to be color the choices you want to or have to make. Epidurals are one of many tools in your labor tool box. Take in this information as something to consider, to know, and to tuck away. To use or not use an epidural can both be right choices.